Is your digestive system not functioning properly? Are you seeing symptoms that include abdominal pain, bloating, constipation, diarrhea, and/or gas?
Those are all signs that you potentially have Irritable Bowel Syndrome (IBS), a common condition when the digestive system doesn’t function properly.
Unfortunately, there’s no definitive diagnosis test for IBS. A combination of factors including history of symptoms, a physical exam and a few tests may be employed before your doctor makes a diagnosis of IBS.
If you think you might have IBS, then this guide will show you if your symptoms fit with a diagnosis of IBS.
- Related article: What is IBS Attack?
Symptoms: When to See a Doctor for Diagnosis
The first step is to make sure you’re experiencing some of the typical symptoms associated with IBS. These symptoms can vary from person to person, but they usually include:
- Abdominal pain or cramping
- Bloating
- Constipation
- Diarrhea
- Gas
- Nausea/Vomiting
If the symptoms have been present for more than 6 months, you should see a doctor.
If you’ve been experiencing recurrent abdominal pain at least once a week in the last 3 months, are any of these true:
- Abdominal pain is related to bowel movements – pain is relieved or worsened by defecation
- Associated with a change in stool form
- Associated with a change in stool frequency
If 2 out of 3 of those are true, you should see a doctor for further diagnosis.

How Does a Doctor Diagnose IBS?
A doctor will likely perform a physical exam, ask questions about your health history, including your family history, symptoms, and their duration. Your doctor may also order blood tests, stool tests, and potentially a variety of other diagnostic tests that we will describe further below.
IBS Types and Symptoms
It is important to determine subtype as IBS treatment recommendations vary based on subtype. There are medications specifically designed for treatment of IBS-C (Constipation predominant IBS) and IBS-D (Diarrhea predominant IBS), although not for IBS-M (IBS Mixed type).
IBS subtype may also change over time, so it’s important for you and your doctors to keep track of stool form and frequency changes.
Doctors will use the Rome IV Criteria’s Bristol Stool Scale to help determine the type of IBS that you have. There are 7 different types of stool on the Bristol Stool Scale:
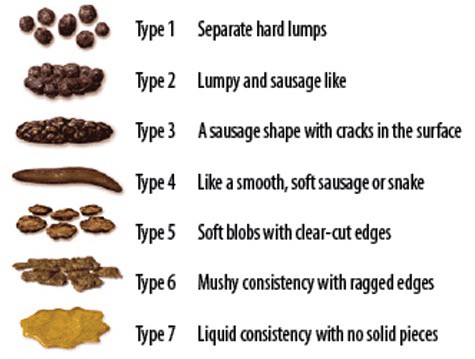
- If over 25% of bowel movements are type 1 or 2 and less than 25% are type 6 or 7, it’s IBS-C
- If over 25% of bowel movements are type 6 or 7 and less than 25% are type 1 or 2, it’s IBS-D
- If over 25% of bowel movements are type 1 or 2 AND over 25% are type 6 or 7, it’s IBS-M
- If none of the above, IBS-U (IBS Undetermined subtype)
In addition to reviewing your symptoms, your doctor will also ask about your family history.
Personal and Family Medical History
Genetics can play a role in IBS occurrence and its severity. If you have a family member who has had IBS, you may be more likely to have or develop IBS.
You may also want to talk to your doctor about other conditions that could cause similar symptoms to IBS.
Your doctor will look for conditions such as Celiac disease, inflammatory bowel disease (IBD), diabetes, thyroid disorders, small intestinal bacterial overgrowth, and other conditions.
They will also review your diet habits, exercise routine, sleep patterns, stress levels, and medication usage.
During your visit, your doctor will also conduct a thorough physical exam. They will look for abdominal tenderness and distension, which may be due to increased gas production.
It can be frustrating for patients who experience chronic abdominal pain and changes in bowel movements without a clear explanation. However, by carefully considering their medical history and conducting a thorough physical exam, doctors can begin to narrow down potential causes and formulate an appropriate treatment plan.
There are unique aspects of IBS in children, which differ in symptom presentation and management strategies compared to adults. For an in-depth understanding of how IBS manifests in younger patients, including specific diagnostic challenges and treatment approaches, refer to our detailed article: Pediatric IBS guide.
Depending on the results of your lab work, your doctor may recommend additional tests. Learn more about risk factors leading to IBS.
10 IBS Diagnostic Tests
There are many ways to diagnose if you have irritable bowel syndrome. Here are some common tests used to help confirm a diagnosis of IBS and exclude other conditions.
1. Stool Test
If you have been diagnosed with IBS, then you will probably have had a stool test done. Stool tests are an important tool for diagnosing IBS. They can help identify the presence of infection, inflammation, or other gastrointestinal problems.
The test involves taking a sample of your stools and testing them for inflammatory markers to look for inflammatory bowel disease, like Crohn’s or ulcerative colitis.
Stool testing for infection is not always needed, but if there is something in the history that suggests this may be infectious (more acute onset, travel, sick contacts) they may check this as well.
Fecal calprotectin and lactoferrin testing are two stool tests that can be used to diagnose IBS. These two biomarkers help in indicating the presence of inflammation in the gut.
Fecal calprotectin is a protein released by neutrophils, white blood cells that accumulate at sites of inflammation, and it’s an indicator of gastrointestinal inflammation. Lactoferrin is also a marker for intestinal inflammation but originates from immune cells known as lymphocytes.
Microbiome analysis has become increasingly popular over time as studies have proven its significance in diagnosing IBS. Gut dysbiosis occurs when there’s an imbalance between good bacteria and bad bacteria in the gut leading to various health issues such as bloating, constipation, diarrhea amongst others.
Microbiome analysis helps determine which bacterial species exist within our guts; this information allows us to create personalized treatment plans for each patient with IBS based on their unique microbiome composition.
2. Colonoscopy
A colonoscopy is a procedure that uses a flexible tube with a tiny camera attached to check the inside of your large intestine. It allows doctors to see any abnormalities in the lining of the colon.
Typically, patients are sedated for this procedure, but it can be done in an unsedated patient as well. Biopsies (small tissue samples) can be obtained for further evaluation by a pathologist looking at the tissue under the microscope.
If there is a history of straining or difficulty evacuating stool in IBS-C, your doctor may want to do a digital rectal exam and possibly further testing called anorectal manometry.
That will help to assess the motor function of the rectum and anus. It tests for other conditions like dyssynergic defecation that can be contributing to evacuation related symptoms and respond to different treatments like biofeedback therapy.
Colonoscopies are also used for cancer screenings. If the patient has any of these alarm features, your doctor may order a colonoscopy to look for IBD and cancer:
- Red or dark blood in stool
- Anemia (low blood counts)
- Unintentional weight loss
- Family history of IBD (Crohn’s or UC) or colon cancer
The colonoscopy will look for IBD/cancer or a source of blood loss.
For patients older than 45 years old, a colonoscopy is recommended regardless of symptoms for age appropriate cancer screening.
If patients are less than 45 years old and they are not improving with standard IBS treatments, the doctor may order a colonoscopy for further diagnosis.
3. Blood Tests
Blood tests are sometimes recommended when you have symptoms of IBS. Blood tests are useful because they help identify potential causes of IBS such as celiac disease, thyroid dysfunction, and anemia. Blood tests may be needed to rule out other diseases and conditions with similar symptoms to IBS.
For example, the doctor can rule out Celiac disease with blood testing if there is concern for IBS-D, as the conditions can have overlapping symptoms of pain, bloating and diarrhea.
Celiac disease is a digestive disorder caused by gluten intolerance; it shares some symptoms with IBS making it difficult to diagnose. Thyroid dysfunction can also cause gastrointestinal issues and affect bowel movements leading to constipation or diarrhea-like symptoms.
Anemia occurs when there’s not enough red blood cells in the body due to iron deficiency which may lead to fatigue, shortness of breath, and abdominal pain.
4. X-ray or CT Scan – Imaging Tests
Imaging tests can also aid in the diagnosis of IBS. X-rays, Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are commonly used for this purpose. These imaging tests provide detailed images of the gastrointestinal tract, allowing physicians to visualize any abnormalities or inflammation that may be present.
An x-ray is a type of imaging test that shows details of the bones, soft tissues, and internal organs. This is a 2 dimensional test.
It can be helpful to evaluate for bowel blockages, constipation, or fecal impaction (a large amount of stool in the rectum).
A CT scan is utilizes X-ray technology to provide cross-sectional images, which allow physicians to interpret them from different angles. By examining these images, gastroenterologists can determine if there are any signs of inflammatory bowel disease like Crohn’s Disease, which has symptoms overlapping with those of IBS.
A CT scan is a 3 dimensional imaging test that can better evaluate solid organs like the liver and pancreas, and the bowel wall for signs of inflammation, which can be seen with Crohn’s, ulcerative colitis or infectious colitis.
An x-ray or CT scan cannot diagnose IBS, but can help rule out other conditions. While imaging tests are not always necessary for diagnosing IBS, they can provide insight into underlying conditions that could be contributing to symptoms. This allows healthcare providers to develop an effective treatment plan tailored specifically for each patient’s needs.
5. MRI
An MRI scan is a non-invasive procedure that uses a powerful magnet and radio waves to create detailed images of organs and tissues within the body. It can help identify structural problems such as tumors or strictures that may be causing IBS symptoms.
MRI scans use radio waves and magnets to create detailed images without using radiation. Doctors use MRI scans to help evaluate liver and pancreas masses, gallstone disease, and cysts in the pancreas.
An MR enterography is sometimes used in the evaluation of Crohn’s disease to assess disease in the small intestine.
| Imaging Modality | Advantages | Disadvantages |
|---|---|---|
| X-ray | Widely available and less expensive than other modalities; useful for evaluating gas patterns and identifying calcifications | Low sensitivity for detecting subtle lesions; limited ability to distinguish between fluid-filled structures |
| CT Scanning | High resolution images allow for detection of small lesions; useful for assessing lymph nodes and surrounding tissue involvement | Radiation exposure; contrast allergy risk; higher cost compared to plain radiographs |
| MRI | Excellent soft tissue contrast without radiation exposure; no need for contrast media in most cases; good for visualizing pelvic organs and liver/biliary tree pathology | Longer scan times than CT scans; higher cost compared to plain radiographs |
6. Upper Endoscopy
Endoscopy is a diagnostic tool that uses a lighted instrument to examine the inside of your stomach and intestines. It allows doctors to view the lining of your esophagus, stomach, and duodenum.
Endoscopic procedures are a valuable tool for diagnosing and treating gastrointestinal disorders. These procedures allow us to view the inside of the digestive tract, take tissue samples, and even perform certain treatments.
Types of endoscopies include upper GI endoscopy, colonoscopy, sigmoidoscopy, and capsule endoscopy. Each type has its own set of risks that must be considered before undergoing the procedure.
For example, upper GI endoscopies carry a small risk of perforation or bleeding while colonoscopies may cause discomfort or injury to the bowel wall. However, these risks are generally low and can be minimized by preparing properly for the procedure.
During an endoscopy, a gastroenterologist inserts a flexible tube called an endoscope into your mouth. Then he or she guides the endoscope down your throat and into your stomach and small intestine.
Biopsies can be obtained to check for things like H. Pylori infection and Celiac disease.
Recovery after an endoscopy is typically quick, but patients should expect some mild discomfort such as bloating or sore throat following upper GI endoscopies.
7. Ultrasound
Ultrasounds are used to evaluate the solid organs in the abdomen like the liver, spleen, pancreas and gallbladder. They do not visualize the stomach and small intestine that well.
Ultrasounds do not involve radiation. They can be limited in obese people.
8. Barium Enema
Barium enemas involve injecting barium, a substance that appears white on x-ray, into your rectum. Your doctor will insert a special tube into your anus and guide it into your lower intestine.
He or she will inject air into the tube so that the barium travels farther into your intestine. The barium gives off a bright white glow under x-ray or fluoroscopy. This can evaluate for things like diverticulosis or strictures (narrowing in the colon).
These are often done in the setting of a failed or incomplete colonoscopy to look for masses or polyps in the unexamined portion of the colon.
9. Capsule Endoscopy
Capsule endoscopy is a newer technology that lets doctors view pictures of your entire gastrointestinal tract without having to pass a probe through your entire digestive system.
This test involves swallowing a pill with a built-in camera. A recorder is worn which remotely captures and stores the images.
The recorder is returned to your doctor and then viewed by the doctor to look for pathology in the small intestine. This can include inflammation, polyps, masses or bleeding spots called arteriovenous malformations.
IBS Diagnosis Final Thoughts
Without a single test that will tell you whether you have IBS or not, a variety of tests may be used to help clarify the diagnosis.
Before going in to see your doctor, it’s also a good idea to keep a food and symptom journal to track the symptoms and pain and discover any foods that may impact your symptoms. It will help you and your doctor with diagnosing IBS.

