Have you ever wondered how liver fibrosis impacts your overall health, or how you can manage it effectively? In our fast-paced lives, discussions about liver health often take a backseat.
However, understanding liver fibrosis, its causes, symptoms, and the latest treatment breakthroughs can be pivotal in safeguarding your well-being.
We’re going to explore the liver’s vital functions, the progression of liver fibrosis to cirrhosis, and the role of diet and lifestyle in managing this condition. We’ll also touch upon the latest research and future directions in liver fibrosis treatment.
Whether you’re someone personally affected by liver fibrosis, or a healthcare professional looking to expand your knowledge, this comprehensive guide will offer valuable insights. So, are you ready to unravel the mysteries of liver fibrosis and equip yourself with the knowledge to lead a healthier life? Let’s embark on this enlightening exploration together.
Liver Fibrosis Key Takeaways
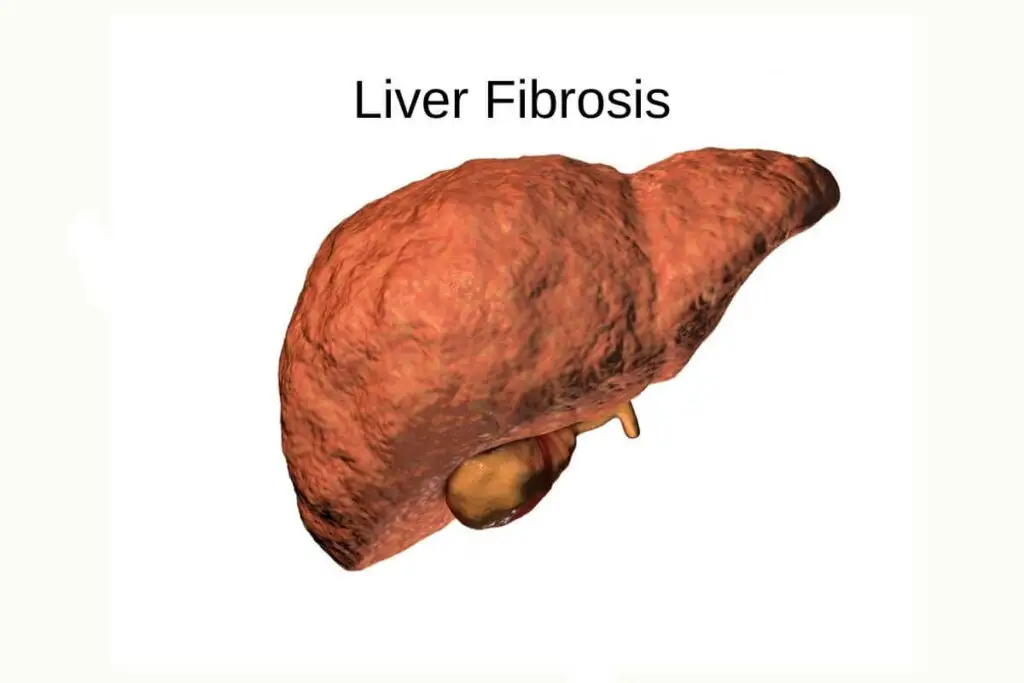
- Liver Fibrosis: The Silent Construction Project in Your Liver Liver fibrosis is the early stage of scarring caused by repeated liver injury, often from conditions like chronic hepatitis or alcohol abuse. Excessive scar tissue formation disrupts the liver’s normal functions, and if left unchecked, can progress to irreversible cirrhosis.
- The Vital Role of the Liver and Its Functions: Your liver performs over 500 crucial functions, including metabolism, detoxification, blood clotting, and bile production. Understanding these functions and supporting liver health is essential for overall well-being.
- Recognizing Liver Fibrosis Symptoms and Early Intervention: Symptoms of liver fibrosis, such as fatigue, abdominal discomfort, and jaundice, may not appear until the condition is advanced. Early detection through regular check-ups and liver function tests can prevent further liver damage.
- Common Causes and Risk Factors for Liver Fibrosis: Alcoholism, viral infections, metabolic disorders, and genetic predisposition are common causes and risk factors for liver fibrosis. Tailoring prevention and treatment strategies to these causes is critical for managing the condition.
- Accurate Diagnosis and Innovations in Liver Fibrosis Treatment: Early and accurate diagnosis of liver fibrosis is key, as it often shows no symptoms until it’s advanced. Innovations in treatment, including enzyme inhibitors and gene therapy, offer promising avenues for managing and potentially reversing liver fibrosis.
- The Progression from Fibrosis to Cirrhosis and Liver Cancer: As liver fibrosis advances, it can lead to more serious conditions like cirrhosis and liver cancer. However, early intervention and lifestyle changes can slow down or even reverse this progression.
- The Role of Diet and Lifestyle in Managing Liver Fibrosis: Moderate coffee consumption, alcohol reduction, weight management through a balanced diet, and regular exercise can all play a significant role in managing liver fibrosis. Lifestyle changes can help support the liver’s natural healing processes and prevent further damage.
What is Liver Fibrosis?
Liver fibrosis is like a silent, underground construction project happening in your liver. It’s the early stage of scarring that occurs when your liver is repeatedly injured, often due to conditions like chronic hepatitis or alcohol abuse.
Now, let’s zoom in on what’s actually happening inside your liver. When faced with injury or inflammation, the liver’s response is to repair itself, much like your body forms a scab on a wound. But in the case of liver fibrosis, this healing process goes into overdrive, leading to excessive scar tissue formation.
Here’s the lowdown: The extracellular matrix, a network of proteins and other molecules, acts as the scaffolding for this scar tissue. Meanwhile, stellate cells, which are normally in a quiescent or resting state, get activated and start producing collagen, the main component of scar tissue.
Why is this important? Well, think of it this way: Your liver is like a factory, with different cells performing specific tasks to keep it running smoothly. When liver fibrosis hits, it’s like a bunch of construction workers have invaded the factory floor, disrupting the whole operation. If this scarring continues unchecked, it can progress to cirrhosis, a more advanced and irreversible stage of liver damage.
So, what can you do? Understanding the causes and risk factors for liver fibrosis, such as chronic viral infections, obesity, and excessive alcohol intake, is key. By making lifestyle changes and seeking early treatment, you can help prevent the progression of liver fibrosis and protect your liver’s vital functions.
In essence, liver fibrosis is a warning sign that your liver is under stress and needs some TLC. By paying attention to this early signal and taking proactive steps, you can potentially prevent more serious liver damage down the line.
Liver Fibrosis Stages Guide
When liver fibrosis is suspected, a doctor will initiate a biopsy procedure, involving a large needle to obtain a liver tissue sample. This sample is crucial for diagnosis.
A pathologist, an expert in disease diagnosis, studies this biopsy under a microscope. Their focus is to understand the level and nature of the liver damage. It’s a challenging process, given the small sample size and potential for different interpretations by various doctors.
Various scales exist to categorize fibrosis stages. These include the Metavir, Ishak, and Batts–Ludwig scales, each assessing the impact on the portal vein (connecting intestines to liver) and the extent and location of fibrous tissue or septa in the biopsy.
The Metavir scoring system quantifies fibrosis progression from A0 to A3:
- A0: No activity
- A1: Mild activity
- A2: Moderate activity
- A3: Severe activity
It also evaluates fibrosis levels from F0 to F4:
- F0: No fibrosis
- F1: Portal fibrosis without septa
- F2: Portal fibrosis with few septa
- F3: Many septa, no cirrhosis
- F4: Cirrhosis
Cirrhosis, the accumulation of scar tissue in the liver, can result from unchecked fibrosis. The most advanced fibrosis stage before cirrhosis in the Metavir system is A3F3.
The Ishak fibrosis scoring system ranges from 0 to 6:
- 0: No fibrosis
- 1: Some portal area expansion, possible short fibrous septa
- 2: Most portal areas expanded, possible short fibrous septa
- 3: Portal area expansion with some portal-to-portal bridging
- 4: Significant portal-to-portal and portal-to-central bridging
- 5: Significant bridging with occasional nodules
- 6: Probable or definite cirrhosis
In the Ishak scale, stage 5 represents the most advanced fibrosis stage before cirrhosis.
The Batts–Ludwig scale, often used in the U.S., grades fibrosis from 0 to 4:
- 0: No fibrosis
- 1: Portal fibrosis
- 2: Occasional portal-to-portal septa
- 3: Fibrous septa
- 4: Definite or probable cirrhosis
Here, stage 3 is the highest fibrosis stage before cirrhosis.
The International Association of the Study of the Liver (IASL) also provides a histological scoring system, dividing chronic hepatitis into four categories:
- Minimal chronic hepatitis
- Mild chronic hepatitis
- Moderate chronic hepatitis
- Severe chronic hepatitis
Additionally, fibrosis staging can rely on tests other than biopsies. For instance, a blood test measuring fibrosis 4 (Fib4) levels can indicate low or high risk for liver fibrosis.
Imaging tests also aid in confirming fibrosis staging. They evaluate liver size, shape, fat content, lumps, or shrinkage. Techniques include:
- Abdominal ultrasound
- Computed tomography (CT) scan of the abdomen
- Magnetic resonance imaging (MRI) scan
- Elastography (combined with ultrasound or MRI)
The Liver: An Essential Organ and Its Functions

Your liver is the unsung hero of your body, tirelessly working behind the scenes like a backstage crew at a rock concert. It’s the largest internal organ and performs over 500 vital functions to keep your body running like a well-oiled machine.
From processing nutrients to detoxifying harmful substances, your liver is a multitasking marvel.
Let’s break it down:
- Metabolism: Your liver is the chief metabolic factory, converting the nutrients from your food into substances your body can use, storing them, or releasing them into your bloodstream as needed. It’s like the ultimate nutrient manager, ensuring your body gets what it needs when it needs it.
- Detoxification: Ever had one too many drinks and relied on your liver to save the day? That’s because your liver is your body’s main detoxifier, breaking down and neutralizing toxins, drugs, and alcohol. It’s like a superhero, swooping in to save the day and keep your body clean and healthy.
- Other Vital Processes: The liver also plays a crucial role in blood clotting, immune system function, and the production of bile, which helps digest fats. It’s like the ultimate multitasker, juggling a variety of essential roles to keep your body in top form.
So, why should you care? Well, your liver’s health directly impacts your overall well-being. When your liver is functioning optimally, your body is better equipped to fight off infections, regulate metabolism, and maintain a healthy balance of nutrients and hormones.
On the flip side, when your liver is compromised – say, by liver fibrosis – it can lead to a cascade of health issues, from fatigue and digestive problems to more serious conditions like cirrhosis and liver cancer.
Understanding the liver’s functions and how to support its health is like giving your body’s MVP the recognition it deserves. By making mindful lifestyle choices and seeking early treatment for liver issues, you’re not just safeguarding your liver but also ensuring that it can continue to work its magic for years to come.
Recognizing Liver Fibrosis Symptoms

Liver fibrosis often creeps in silently, like a ninja in the night. But as it progresses, your body might start sending out distress signals. These can vary from mild to more pronounced, depending on the stage of fibrosis and your individual health.
Here are some common liver fibrosis symptoms to watch out for:
- Fatigue: Feeling tired all the time, even after a good night’s sleep.
- Abdominal discomfort: A dull ache or feeling of fullness in the upper right side of your abdomen.
- Unexplained weight loss: Dropping pounds without trying.
- Loss of appetite: Not feeling hungry, even when you haven’t eaten.
- Jaundice: Yellowing of the skin and eyes.
- Swelling in the legs and abdomen: Known as edema, it can be a sign of advanced fibrosis.
Why is early symptom identification so crucial? If you catch liver fibrosis in its early stages, you have a better chance of preventing it from progressing to more serious conditions like cirrhosis or liver cancer.
Your liver is a hardworking organ, but it’s also a bit shy. It doesn’t like to show its cards until things get really serious. So, it’s up to you to pay attention to the whispers of discomfort your liver might be sending out.
If you’re experiencing any of these symptoms, don’t brush them off as just a bad day. It’s worth getting them checked out. Early detection not only helps in preventing further liver damage but also gives you a head start on making lifestyle changes that can support your liver health.
Remember, your liver is like a quiet superhero, working tirelessly behind the scenes. It’s time to be its sidekick and listen to what it’s trying to tell you.
Common Causes of Liver Fibrosis

Liver fibrosis can be triggered by a myriad of factors, some of which are more common than others. Here’s a quick rundown of the major players:
- Alcoholism: The liver is a superhero at processing toxins, but excessive alcohol consumption can overwhelm its superpowers, leading to liver damage and eventual scarring, aka fibrosis.
- Viral Infections: Hepatitis B and C are the usual suspects here. These viral hepatitis infections can cause chronic liver inflammation, which gradually progresses to fibrosis.
- Metabolic Disorders: Type 2 diabetes and obesity can create a perfect storm in your liver. Insulin resistance, high blood sugar, and a build-up of fat in the liver cells all contribute to fibrosis.
So, what’s the big deal with all these causes? Well, they all set off a chain reaction of liver inflammation and injury. Over time, this constant wear and tear leads to the formation of scar tissue, which impairs liver function.
It’s like a road that’s constantly under construction. At first, a few potholes here and there aren’t a big deal. But as time goes on and more patches are laid down, the road becomes less and less smooth, making it harder for traffic to flow.
Understanding these causes is crucial because it helps us tailor our prevention and treatment strategies. For instance, if alcohol is your liver’s nemesis, cutting back or quitting altogether can dramatically slow down or even reverse fibrosis.
Similarly, managing your weight and blood sugar levels can go a long way in preventing or slowing the progression of liver fibrosis if you have a metabolic disorder.
In a world where liver fibrosis is often a silent condition, knowing its common causes can empower you to take charge of your liver health.
Risk Factors for Liver Fibrosis

Liver fibrosis is often the result of ongoing liver damage, and certain factors can increase your risk. Let’s take a peek at what could be raising your liver’s eyebrows:
- Genetic Predisposition: You know how families have that one trait that’s passed down from generation to generation? Well, liver health can be one of them. If you have a family history of liver disease, you might want to keep an extra close eye on your liver health.
- Viral Infections: Viral hepatitis B and C are the common enemies of healthy liver cells. Chronic infections with these viruses can lead to liver inflammation and scarring, the primary drivers in the progression of fibrosis.
- Autoimmune Diseases: Your immune system is like a protective army, but in autoimmune diseases, it turns against your own body, including your liver. Conditions like autoimmune hepatitis and primary biliary cholangitis can contribute to liver fibrosis.
- Alcohol and Drug Abuse: A little indulgence is okay, but excessive alcohol consumption and certain drugs can wreak havoc on your liver, leading to fibrosis over time.
- Obesity and Metabolic Syndrome: The liver plays a key role in metabolism, and when it’s overwhelmed by fat or insulin resistance, it can lead to inflammation and scarring.
- Other Chronic Conditions: Conditions like non-alcoholic fatty liver disease (NAFLD), hemochromatosis (excess iron in the body), and Wilson’s disease (copper accumulation) can also up your fibrosis risk.
Understanding these risk factors is the first step in taking control of your liver health. If you have a family history of liver disease, have been diagnosed with a viral infection, or are struggling with an autoimmune condition, it’s essential to work with your healthcare team to monitor and manage your liver health.
Diagnosing Liver Fibrosis Accurately

The first step in managing liver fibrosis is nailing down the diagnosis. Your liver’s like the quiet kid in the back of the classroom – it doesn’t always announce when something’s wrong. But we have ways to coax the truth out of it.
- Liver Function Tests: These are your starter tests, like ALT and AST, that give a general picture of how your liver is functioning. Tests will include a physical exam and blood tests. They’re like the first few bites of a meal – they give you a taste but not the full story.
- Imaging Techniques: Image tests are where the party gets interesting. We have some fancy tools that can give us a closer look at your liver, like MRI and transient elastography. MRI is like the high-resolution camera of the medical world, while transient elastography measures liver stiffness, a key indicator of fibrosis.
- Magnetic Resonance Elastography (MRE): This is the new kid on the block, and it’s making waves. MRE combines MRI (Magnetic Resonance Imaging) with sound waves to create a detailed map of liver stiffness. It’s like the Google Earth of liver imaging – you can zoom in and see everything.
- Liver Biopsy: This procedure is considered the definitive method for both the diagnosis and the grading of the extent of hepatic fibrosis, as well as pinpointing the specific liver condition responsible for the fibrosis.
Despite its status as the benchmark for diagnosis, a liver biopsy is not without its risks. Patients may experience minor adverse effects, such as discomfort following the procedure, with a prevalence ranging from 10 to 20%. More concerning, however, are the serious complications, which can occur in 0.5 to 1% of cases, including significant hemorrhage. That’s why imaging tests are often used iniitally.
Another challenge with liver biopsy is the inherent variability in the procedure itself. A sample of liver tissue may not accurately represent the condition of the entire organ due to sampling error. Additionally, even when normal liver tissue is obtained, the interpretation of histological results can be subjective, leading to variations among different observers.
Why is accurate diagnosis so important? Well, think of it this way: the earlier we catch liver fibrosis, the more we can do to slow it down or even reverse it. Accurate diagnosis guides your treatment plan, helping you and your healthcare team make informed decisions.
So, if you suspect liver issues or have risk factors like obesity or excessive alcohol use, don’t play the waiting game. Get those liver function tests and imaging studies done. Your liver will thank you for it.
Innovations in Liver Fibrosis Treatment

The landscape of liver fibrosis treatment is undergoing a revolution, and the future looks promising. We’re not just talking about the traditional medications, but also lifestyle changes and even potential gene therapies.
- Enzyme inhibitors – They offer targeted therapy that specifically hones in on the processes driving liver scarring. These inhibitors act like precision tools, halting the fibrosis process in its tracks.
- Gene therapy – A field that’s been making waves in various medical arenas, is also showing potential in the treatment of liver fibrosis. By targeting specific genes involved in fibrosis, this therapy offers a more direct and personalized approach to treatment.
- Lifestyle changes – While not as flashy as gene therapy, adopting a liver-friendly diet, exercising regularly, and avoiding alcohol and certain medications can significantly slow down the progression of liver fibrosis.
The bottom line: the future of liver fibrosis treatment isn’t just about popping pills. It’s about a holistic approach that involves both cutting-edge medications and lifestyle modifications.
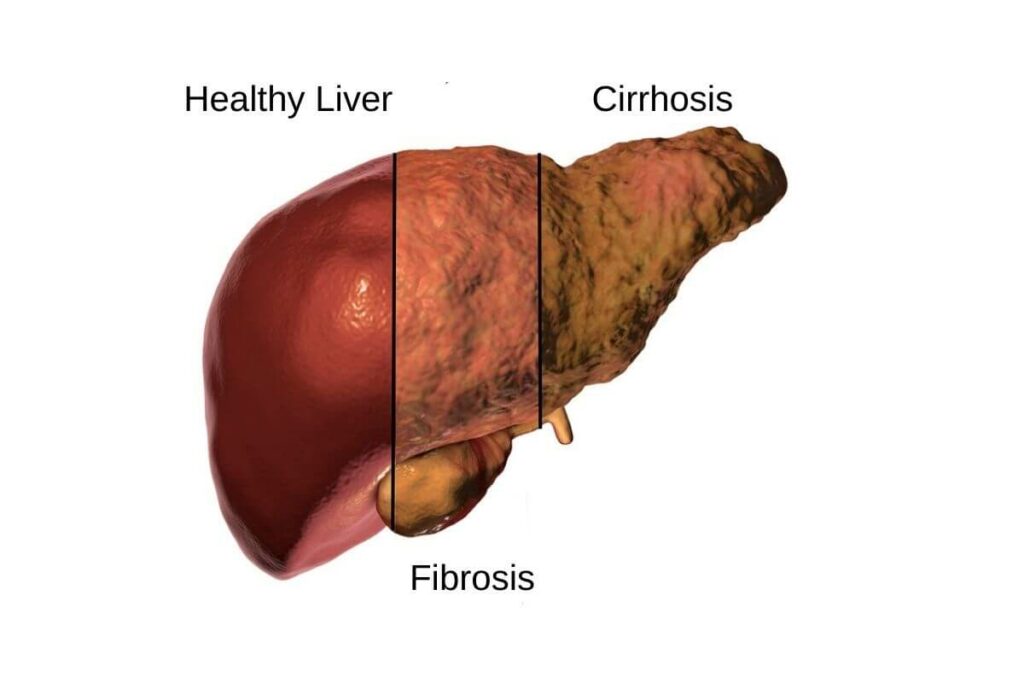
The Progression: From Fibrosis to Cirrhosis and Beyond
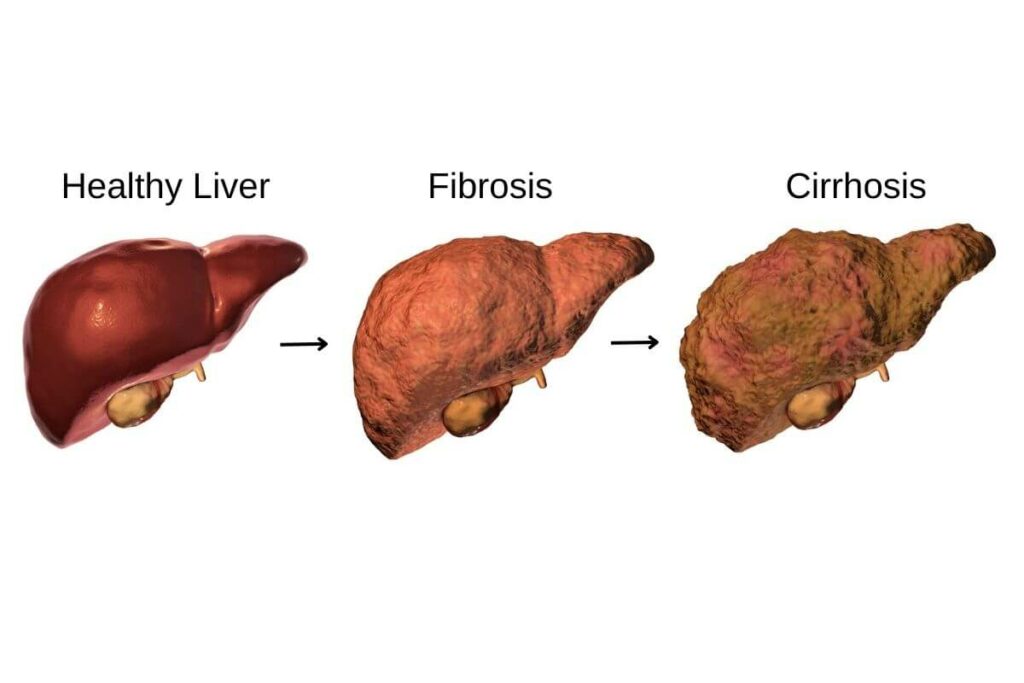
As liver fibrosis advances, it can lead to more serious conditions, such as cirrhosis and even liver cancer. When scar tissue builds up in the liver due to prolonged inflammation, it can impair liver function and blood flow. This is the tipping point where severe fibrosis has transitioned to cirrhosis and liver failure.
Now, cirrhosis isn’t a reversible condition. It’s like trying to unscramble an egg – once the liver is significantly scarred, it’s hard for it to function normally again. The liver becomes nodular and lumpy, and its ability to filter toxins and produce vital proteins is severely compromised.
Cirrhosis isn’t just a roadblock; it’s also a red flag for liver cancer. According to the American Cancer Society, people with cirrhosis have a higher risk of developing liver cancer. So, it’s like a domino effect – one condition can lead to another.
Here’s the silver lining: early intervention can slow down, and in some cases, even reverse the progression from fibrosis to cirrhosis. Lifestyle changes, such as a healthy diet and exercise, and treating the underlying cause of liver damage, like hepatitis, can make a world of difference.
And let’s not forget about the power of regular check-ups. Liver function tests and imaging studies can help catch liver fibrosis in its early stages, giving you a head start on preventing its progression. So, if you know you’re at risk, or if you’ve been diagnosed with liver fibrosis, don’t skip those doctor’s appointments.
Remember, the liver is a remarkable organ, but it needs a little TLC to keep doing its job. By understanding the stages of liver fibrosis and the potential risks, you’re already one step ahead in protecting your liver health.
Learn more in the Liver Cirrhosis Guide.
The Role of Diet and Lifestyle in Managing Liver Fibrosis

Your diet and lifestyle can play a significant role in managing liver fibrosis. Here’s the lowdown on what you can do:
- Caffeine: Good News for Coffee Lovers
- Research suggests that moderate coffee consumption can actually be beneficial for liver health. Caffeine has been linked to a lower risk of fibrosis progression in individuals with chronic liver disease. So, feel free to savor that morning cup of joe or green tea.
- Alcohol Reduction: A Vital Step
- This one’s a no-brainer. Cutting back on or eliminating alcohol is crucial for managing liver fibrosis. Even small amounts of alcohol can exacerbate liver damage. If you’re finding it tough, consider seeking support from friends, family, or a professional.
- Weight Management: The Power of a Balanced Diet
- Maintaining a healthy weight through a balanced diet and regular exercise is key. Excess weight can lead to fatty liver disease, which can then progress to fibrosis. Aim for a diet rich in fruits, vegetables, lean proteins, and whole grains.
- Lifestyle Modifications: Stress Less, Sleep More
- Chronic stress and poor sleep can impact liver health. Consider incorporating stress-reducing practices like yoga, meditation, or simply taking time for hobbies you enjoy. Also, ensure you’re getting adequate, quality sleep each night.
- Nutritional Supplements: The Devil’s in the Details
- Some studies have shown that certain nutritional supplements, like vitamin E, may have potential benefits in managing liver fibrosis. However, always consult with your healthcare provider before starting any new supplements.
Remember, while these lifestyle and dietary changes can help manage liver fibrosis, they’re not a substitute for medical treatment. Always consult with your healthcare provider to create a comprehensive plan that’s tailored to your individual needs.
Complications and Comorbidities Associated with Liver Fibrosis

Liver fibrosis isn’t an isolated issue; it’s like a domino effect that can knock down other aspects of your health. Here’s the lowdown:
- Portal Hypertension: As your liver becomes scarred, blood flow through it is impeded, leading to increased pressure in the portal vein. This can result in serious complications like varices (enlarged veins) and ascites (fluid buildup in the abdomen).
- Hepatic Encephalopathy: When the liver can’t effectively detoxify the blood, toxins can affect brain function, leading to confusion, personality changes, and in severe cases, coma.
- Cardiovascular Diseases: Research suggests that liver fibrosis is linked to an increased risk of heart disease. The exact reasons for this connection are still being unraveled, but it’s a good reminder to take care of your ticker too.
- Diabetes: There’s a bidirectional relationship between liver fibrosis and diabetes. Having diabetes can exacerbate liver fibrosis, and vice versa. It’s a complex dance that needs careful management.
Liver fibrosis is not just about the liver; it’s about your whole body. That’s why it’s crucial to address it comprehensively, considering its potential impact on other organ systems.
So, if you’re managing liver fibrosis, it’s not just about the liver; it’s about your whole body. Keep an eye on your heart health, blood sugar, and overall well-being. And as always, work closely with your healthcare team to navigate these interconnected health challenges.
Living with Liver Fibrosis: Patient Support and Resources

Navigating a liver fibrosis diagnosis can be overwhelming, but you’re not alone in this journey. Patient support networks and advocacy groups are lifelines for individuals living with liver fibrosis. These communities offer a wealth of knowledge, emotional support, and practical advice that can make a significant difference in your quality of life.
Here’s how patient support and advocacy groups can help you:
- Emotional Support: Sharing your experiences with people who understand what you’re going through can be incredibly comforting. It can help you feel less isolated and more empowered in managing your condition.
- Educational Resources: These groups often provide access to the latest information on liver fibrosis, treatment options, and lifestyle tips. Knowledge is power, and staying informed can help you make better decisions about your health.
- Practical Guidance: From managing medication side effects to navigating insurance and financial assistance, these groups can offer invaluable practical advice.
- Professional Support: In addition to patient networks, it’s essential to have a strong healthcare team on your side. A gastroenterologist or hepatologist can provide tailored medical advice, while a registered dietitian can help you create a liver-friendly diet plan.
Here are some reputable resources to consider:
- American Liver Foundation: Offers support services, educational materials, and local support groups.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Provides comprehensive information on liver diseases and treatment options.
- Liver Foundation: Offers a variety of resources, including a liver helpline, support groups, and educational materials.
- Your Healthcare Provider: Don’t underestimate the value of your healthcare team. They can provide personalized guidance and referrals to local resources.
Remember, living with liver fibrosis is not just about managing the physical symptoms, but also about finding the emotional and social support you need. By reaching out to patient support networks and leveraging professional resources, you can navigate this journey with greater confidence and resilience.
Final Thoughts and Next Steps in Your Liver Fibrosis Journey
In your journey to understand liver fibrosis, you’ve delved into its causes, symptoms, and the latest breakthroughs in treatment. Here are the key takeaways to keep in mind as you move forward:
- Lifestyle Modifications Matter: Whether it’s cutting back on alcohol, managing your weight, or controlling your blood sugar, simple lifestyle changes can have a profound impact on liver health.
- Regular Monitoring is Key: If you have risk factors for liver fibrosis or have been diagnosed with an early stage, regular check-ups and monitoring of liver function can help catch any progression early.
- Consult with a Specialist: Don’t hesitate to consult a hepatologist or gastroenterologist. They can provide personalized advice and a treatment plan tailored to your specific condition.
- Stay Informed About New Treatments: The landscape of liver fibrosis treatment is rapidly evolving, with new medications and therapies on the horizon. Stay informed and discuss these options with your healthcare provider.
- Support Your Liver: Certain supplements and dietary changes can support liver health. Always consult with your healthcare provider before making any significant changes to your diet or starting a new supplement regimen.
Your next steps should include scheduling an appointment with a healthcare provider to discuss the best approach for your liver health. Remember, you’re not in this alone. There’s a wealth of information and support available to you as you navigate your liver fibrosis journey.
By taking proactive steps and working in tandem with your healthcare provider, you can manage liver fibrosis effectively and improve your quality of life. So, as you move forward, make your health a priority and let the knowledge you’ve gained empower you on this journey.
- https://www.cancer.org/cancer/types/liver-cancer/causes-risks-prevention/risk-factors.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8700445/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7438353/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721971/table/T2/
- https://www.cdc.gov/nchs/fastats/liver-disease.htm
- https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis/symptoms-causes
- https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/treatment
- https://liverfoundation.org/about-your-liver/how-liver-diseases-progress/
