You cannot live without a properly functioning liver. About 26,000 Americans die each year of cirrhosis (liver failure), making it the 12th leading cause of death in the United States.
The most common cause of cirrhosis is chronic alcoholism, which accounts for approximately 40% of the 26,000 people who die from the disease.
The liver works to keep us healthy, converting food into substances needed for life and growth, and storing glycogen, amino acids, protein, and fat. It also produces the enzymes and bile that help digest food, neutralizes toxins in our blood, and produces immune agents to control infection.
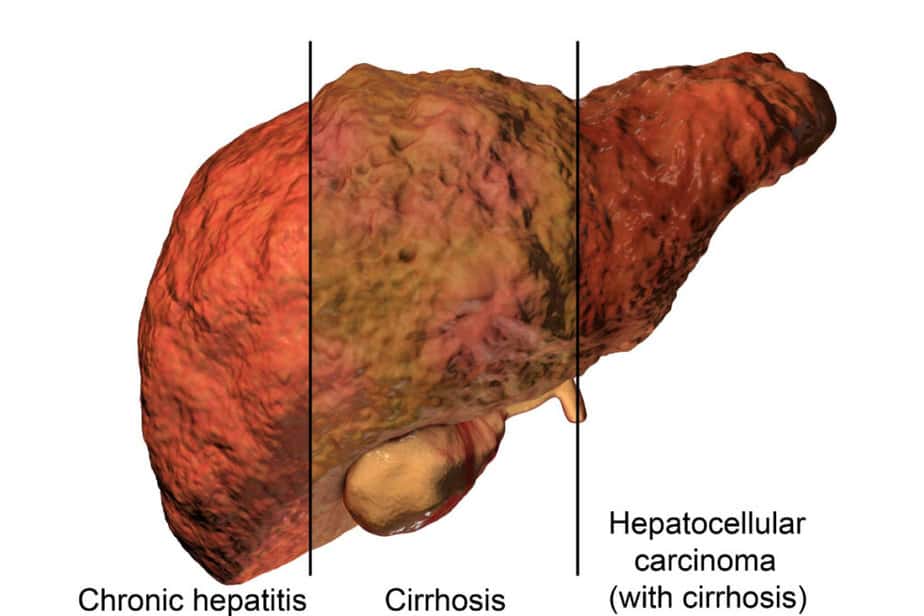
Liver fibrosis is a condition where scar tissue builds up inside your liver over time. This scarring can lead to cirrhosis if you have long-term damage to your liver.
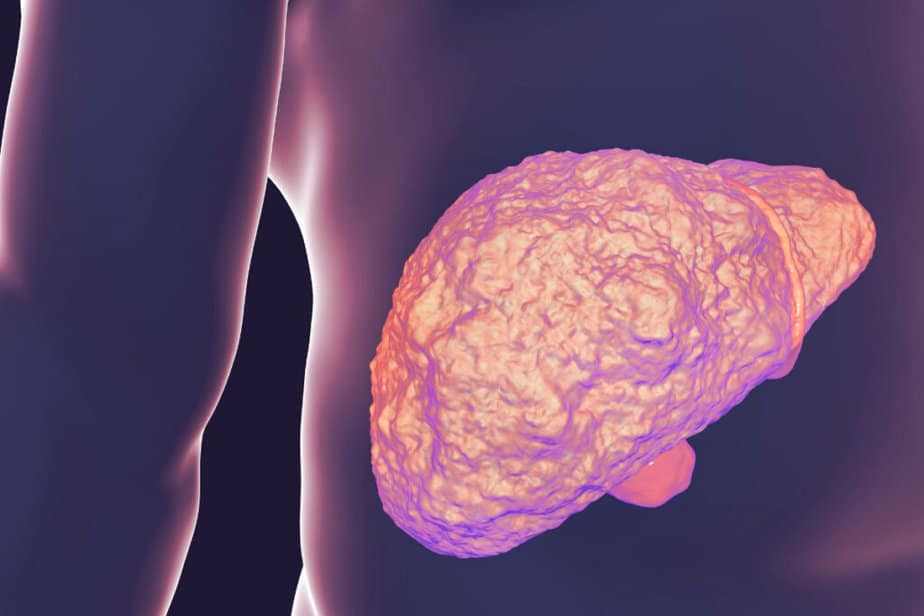
When cirrhosis sets in, liver scarring begins to replace healthy tissue and the result is a hardened liver. The scar tissue blocks the flow of blood through the liver, preventing the organ from functioning properly.
In this article, we will explore the common symptoms, causes, and treatment options for liver cirrhosis in order to help you gain control over your health and well-being.
What is Cirrhosis?
Cirrhosis is a condition that affects the liver, causing it to become scarred and damaged over time. This damage can result in many different symptoms, including jaundice, fatigue, abdominal pain, and more.
The liver is an essential organ in our body, responsible for a variety of functions such as detoxification, metabolism, and storage of nutrients. Maintaining liver health is crucial to ensure optimal bodily function.
Prevention is always better than cure when it comes to liver diseases. It’s important to keep your weight under control, avoid excessive alcohol intake, and get vaccinated against Hepatitis A & B infections. Incorporating exercise into your daily routine can also make a significant difference.
If you’re already living with chronic conditions that could affect your liver health like diabetes or high cholesterol levels, managing them effectively can go a long way in keeping your liver healthy.
Cirrhosis Causes
Liver cirrhosis is a serious and debilitating condition that affects millions of people worldwide. The causes of cirrhosis are varied and complex, but chronic alcoholism and hepatitis C are the most common causes of cirrhosis in the United States. NASH (non-alcoholic steatohepatitis) is also rapidly becoming a leading cause.
Other causes include:
- Alcoholic liver disease symptoms
- Autoimmune hepatitis
- Blocked bile ducts
- Chronic hepatitis B
- Chronic hepatitis C
- Exposure to toxins such as alcohol, certain drugs, and infections
- Inherited illnesses such as alpha-1 antitrypsin deficiency, hemochromatosis, Wilson’s disease, galactosemia, and glycogen storage diseases
- Nonalcoholic steatohepatitis (NASH)
- Prolonged exposure to environmental toxins such as arsenic
Men tend to develop cirrhosis of the liver more often than women. While liver cirrhosis can be caused by a variety of factors, including alcohol abuse, viral hepatitis, and fatty liver disease, all cases share similar symptoms that should not be ignored.
Cirrhosis Symptoms and Complications
During the early stages, many people with cirrhosis experience no symptoms. Liver cirrhosis can be difficult to detect in its early stages because symptoms may not appear until significant damage has been done to the liver.
However, as scar tissue replaces healthy cells, and liver function begins to fail, a person may experience a variety of symptoms and complications:
- Abnormal accumulation of fluid in the abdominal cavity (ascites)
- Bleeding from engorged veins (varices) in your esophagus or stomach
- Dark urine
- Easy bruising
- Fatigue
- Impotence
- Itching hands and feet
- Kidney dysfunction
- Lack of appetite
- Liver cancer (Early signs of liver cancer)
- Liver failure
- Loss of interest in sex
- Muscle wasting or loss
- Nausea
- Osteoporosis/osteopenia
- Portal hypertension (an increase in blood pressure in veins that carry blood from the abdominal organs to the liver)
- Small, spider-like blood vessels under the skin
- Swelling of legs and feet from retained fluid (edema)
- Hepatic encephalopathy (forgetfulness, confusion, trouble concentrating, change in sleeping habits, behavioral, personality, and mood changes)
- Yellowing of skin and eyes (jaundice and icterus)
If you have any of these symptoms, it’s important to see your doctor as soon as possible for proper diagnosis and treatment. Preventative measures such as avoiding excessive alcohol consumption and maintaining a healthy diet and exercise routine can help reduce your risk of developing liver cirrhosis.
If you or someone you love is experiencing unexplained fatigue or abdominal discomfort, it may be time to seek medical attention.
Cirrhosis Screening and Diagnosis
In addition to a personal history and physical examination, various testing methods are used to diagnose cirrhosis:
- Blood tests – blood count, liver enzymes, renal function, coagulation factors.
- Computerized tomography (CT scan) – to look for nodularity or a shrunken liver as well as complicates like fluid build up or varices – dilated veins.
- Magnetic resonance imaging (MRI) – use magnetization and radio waves to produce images of the internal organs to get a picture of the liver.
- Ultrasound – high-frequency sound waves are bounced off internal tissue, and their echoes converted into images.
- Liver biopsy – able to look for inflammation, signs of what caused liver disease, and evaluate the degree of fibrosis or scarring.
Regular check-ups with your doctor along with appropriate detection methods such as blood tests and imaging scans can aid in early detection and management of the disease. Don’t wait until it’s too late – take control of your health today by taking preventative measures and seeking medical attention if needed.
Imaging studies are crucial in the diagnosis and evaluation of liver cirrhosis. These tests provide valuable information about the extent of damage done to your liver and help us determine the most appropriate treatment approach for your condition.
When it comes to imaging, two commonly used techniques are MRI and CT scan. Both these scans use contrast agents to highlight different structures within your body. However, while an MRI is more detailed and provides better soft tissue resolution, a CT scan is quicker and less expensive. Both tests help to get a complete picture of what’s going on inside your liver.
Cirrhosis Care and Treatment
While liver damage from cirrhosis is permanent and irreversible, treatment can help to delay the progression of the disease, as well as reduce the likelihood of developing complications. Treatment is dependent upon the cause, and is designed to address any complications a patient may be experiencing.
Regardless of the cause, abstaining from alcohol and following a healthy diet are essential. Nutrition plays a key role in therapy because cirrhosis sufferers are often malnourished. A high-calorie, high-protein, nutrient-dense diet can help liver cells to regenerate.
Restricted salt intake is advised as salt causes water retention. The avoidance of raw shellfish and oysters is recommended as they may contain bacteria that can cause severe infection.
Limiting medications is usually advised because a damaged liver is unable to properly detoxify itself of drugs. Avoid aspirin and other non-steroidal anti-inflammatories such as ibuprofen and naproxen. Tylenol should also be limited to no more than 2 grams in a day.
Because liver damage has an effect on immune functioning, it’s wise to keep up with vaccinations such as those for hepatitis A and B, influenza, and bacterial pneumonia.
When your liver is damaged, it is a good idea to avoid contact with people who are ill since the immune system is not functioning at its optimum.
Proper nutrition plays a key role in managing symptoms and slowing progression. Ask your health care provider about multivitamins and other supplements. For example, omega 3 fatty acids (found primarily in fish, fish oils, flax, flaxseed oils, and walnuts) are believed to provide protection for the liver.
Physical activity is important to help prevent deconditioning and loss of muscle mass.
Sometimes complications from cirrhosis cannot be controlled, and/or the liver becomes so damaged from scarring that it ceases to function. In these cases, a liver transplant is necessary and is the only method to overcome cirrhosis of the liver.
Lifestyle changes are an integral part of managing cirrhosis effectively.
Lifestyle Changes For Managing Cirrhosis
Eating a healthy, balanced diet, getting regular exercise, managing stress levels, and reducing alcohol consumption are all key lifestyle changes for Cirrhosis patients.
Eating plenty of fresh fruits and vegetables, lean proteins, and whole grains can help maintain a healthy weight and improve energy levels.
Additionally, reducing alcohol consumption and managing stress through activities such as yoga or meditation can help to reduce the symptoms of Cirrhosis.
Healthy dieting also does not mean sacrificing all your favorite foods either. Balanced nutrition plays an enormous role in maintaining good health while living with liver cirrhosis.
When dealing with such a condition, consuming a well-rounded diet high in protein and low in sodium can aid in preventing further damage to the liver.
In addition, incorporating vegetables and fruits into one’s daily meals provides essential vitamins and minerals necessary for overall body function.
It is worth noting that alcohol intake must cease immediately as it exacerbates any pre-existing symptoms associated with liver cirrhosis.
Dietary restrictions vary depending on the severity of one’s condition, but some general recommendations include limiting salt intake, avoiding processed or fatty foods, and monitoring fluid consumption carefully.
These limitations aim at reducing inflammation within the liver while also promoting healthy digestion by easing stress on other organs such as the pancreas and kidneys.
Remember always to consult a dietician or physician before making significant dietary changes.
Ultimately, taking control of one’s eating habits helps manage symptoms related to liver cirrhosis effectively without compromising taste preferences.
Check out these other liver conditions to learn more:
- What is Gilbert’s Disease?
- Hepatitis C Symptoms
- Can Milk Thistle Protect Your Liver From Disease?
- What are Gallstones?
- High Liver Enzymes Causes
Liver Cirrhosis FAQs
Can Liver Cirrhosis Be Cured?
Liver cirrhosis cannot be cured completely. However, there are treatment options available to manage the symptoms and slow down the progression of the disease.
In some cases, a liver transplant may be necessary for advanced stages of cirrhosis.
Alternative therapies such as herbal supplements or acupuncture have not been scientifically proven to cure cirrhosis but may provide additional support in conjunction with medical treatments prescribed by your doctor. It’s important to remember that managing cirrhosis requires ongoing care and attention, but with proper treatment and lifestyle changes, individuals can still lead fulfilling lives.
What Is The Role Of Diet In Managing Liver Cirrhosis?
Dietary restrictions play a crucial role in managing liver cirrhosis. It’s best to alcohol and high-fat meals as they may worsen the condition.
It is also important to limit salt intake to prevent fluid retention, which can lead to complications such as ascites or edema.
Nutritional supplements like vitamins and minerals are highly recommended to improve overall health, but must only be taken after consulting with a healthcare professional.
With proper diet management, individuals with liver cirrhosis can have better control over their condition and potentially reduce the risk of further liver damage.
Does Liver Cirrhosis Always Lead To Liver Failure?
Liver cirrhosis is a serious condition that can lead to many complications, including liver failure. However, it’s important to note that not all cases of liver cirrhosis will progress to this stage.
Prognosis and complications vary depending on the individual case, but early detection of liver cirrhosis can greatly improve outcomes. Regular check-ups and screenings are important for those at risk of developing liver diseases.
By taking control of your health through preventative measures and seeking medical attention when needed, you can help manage the progression of liver cirrhosis and potentially avoid more severe complications such as liver failure.
Can Liver Cirrhosis Be Prevented?
Prevention strategies for liver cirrhosis involve lifestyle modifications that can significantly reduce the risk of developing this condition.
Maintaining a healthy weight through regular exercise and a balanced diet prevents fatty liver disease, which is one of the leading causes of cirrhosis.
Additionally, avoiding excessive alcohol consumption and practicing safe sex are crucial in preventing viral hepatitis infections that can lead to cirrhosis.
It’s important to take control of your health by making these simple but impactful changes to your daily routine.
How Long Does It Take For Liver Cirrhosis To Develop?
Liver cirrhosis is a progressive disease that can take years to develop. In fact, studies have shown that it can take up to 10-20 years for the liver to become severely damaged and for symptoms of cirrhosis to appear.
However, this timeline varies depending on various risk factors such as alcohol consumption, hepatitis C infection, and obesity. Be mindful of these risk factors and make necessary lifestyle changes in order to prevent or delay the progression of liver cirrhosis.
It’s important to remember that while prevention may not always be possible, taking control of one’s health can greatly impact the timeline of the disease’s development.
- https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis
- https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis/definition-facts
- https://medlineplus.gov/cirrhosis.html
- https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=85&ContentID=P00662
- https://www.meddean.luc.edu/lumen/meded/orfpath/cirhosis.htm
- https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/cirrhosis

